The expression “time is brain” has long been used in stroke education materials to convey the importance of urgency when treating stroke patients. The phrase is credited to Dr. Camilio Gomez, a stroke specialist at Loyola Medicine, who used this phrase in a 1993 editorial to emphasize the importance of time in stroke therapy. In a recent paper, Dr. Gomez observed that “the effect of time on the ischemic process is relative”[1] because of the improvements in imaging technologies and available therapies.
Yet time still matters, and time savings through quality diagnostics are as essential as ever in stroke treatment. Artificial intelligence (AI) in medical image analysis is making a difference in the speed and accuracy of the information available to the stroke team. Rather than time being the only factor, detailed information about the brain tissue that might still be saved can give stroke teams more options than were previously available[2].
What is a Stroke?
Fast and accurate diagnostics are essential in making critical decisions on the course of treatment. Time saved in the first few hours—even by a few minutes—can make a significant difference to the patient’s survival and quality of life.
Diagnosing Stroke: Signs and Symptoms
- Face drooping
- Arm weakness
- Speech difficulty
- Time to call emergency medical services and note the time of onset
According to the American Health Association, it is better to call an ambulance than to drive to the hospital if a stroke is suspected. Some ambulances are equipped to perform diagnostics en route to the hospital and may be able to expedite getting the stroke patient treated appropriately at the nearest qualified center.
Levels of Stroke Care
The following four-stroke certifications are most commonly used in the United States, listed from the most basic to the most advanced:
- Acute Stroke Ready Hospitals provide diagnostic imaging to distinguish between hemorrhagic and ischemic strokes. They can administer thrombolytic drugs to eligible patients. After a patient receives treatment, they are transferred to another center better able to monitor stroke patients
- Primary Stroke Centers have dedicated stroke beds and can provide monitoring after thrombolytic therapy and have more advanced medical imaging
- Thrombectomy-capable Stroke Centers add the ability to do mechanical thrombectomies, neuro-intensive care, and provide 24×7 onsite critical care
- Comprehensive Stroke Centers offer the highest level of care with a team of specialists capable of supporting the most complex cases, and also have a research mission
- Stroke Units (SU) provide basic care including IV thrombolytic care, neuro-intensive care, and the ability to treat early complications
- Stroke Centers (SC) offer thrombectomy and other neuro-radiological and surgical interventions in addition to SU capabilities
Key Clinical Decisions in Acute Stroke Treatment
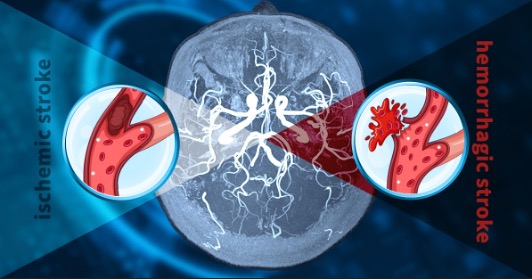
One of the first critical decisions is to confirm the stroke diagnosis versus other conditions mimicking strokes, such as hypertensive encephalopathy, medication-induced neurologic deficits, and hypoglycemia. A key early decision that informs the treatment of stroke depends in part on whether the reduction in blood supply to the brain is due to a narrowing of a blood vessel (ischemia) or from a ruptured blood vessel (hemorrhage). Ischemic strokes are the most common type of stroke, accounting for roughly 87% of all strokes in the United States alone. However, hemorrhagic strokes tend to be more severe with higher short-term mortality as compared with ischemic strokes. In some cases, hemorrhagic strokes can be treated surgically.
- Thrombolysis: A reperfusion therapy in which drugs are used to cause a breakdown (called “lysis”) in the clot. Alteplase is the most commonly used IV-tPA drug. Many hospitals set target times such as 60 minutes from “Door to Needle” (DTN) for patients on this pathway
- Endovascular Interventions which are minimally invasive procedures, such as mechanical thrombectomy (MT), used to remove clots via catheters within blood vessels large enough and accessible for the procedure, such as Large Vessel Occlusions (LVOs)
The potential benefit or risk to the patient for these therapies is largely informed by diagnostic imaging. This often involves the visualization and quantification of data from medical images regarding the salvageable brain tissue.
Referrals for Endovascular Therapy
- Intra-arterial Thrombosis is used with patients with contraindications for IV-tPA. These doses are administered under direct visualization by the interventionist to limit the dose or to locally concentrate the dose
- Mechanical Thrombectomy is a minimally invasive procedure using a microcatheter and other devices to trap and remove the clot from an occluded artery. The microcatheter is inserted in the groin and advanced up through the neck and into the brain. The interventionists can then extract the clot from the blood vessel, sometimes hours after the stroke onset. This is another opportunity for AI, algorithms that can automatically process head CTAs and notify stroke teams when LVO is suspected in a scan
Several clinical trials have shown that endovascular therapies for AIS have the potential for extending the time window for effective treatment of stroke within six hours of stroke onset, and even beyond the six-hour time window in a highly selected population using CT perfusion or MR perfusion[5]. The MR CLEAN-LATE study protocol for a randomized controlled trial was published in February 2021 and aims to assess the safety and efficacy of EVT for patients treated from 6 to 24 hours last known well after selection based on the presence of collateral flow. Patient inclusion in this multi-center phase III trial began in January 2018.
AI for Stroke Detection
Software medical devices using deep learning can process the DICOM images from these modalities within minutes. For example, CuraRad-ICH, Keya Medical’s ICH detection algorithm, has an average response time of 43 seconds from receipt of a non-contrast head CT to notification of the presence of brain bleeding.
Because of the speed, visualization, and measurement capabilities of well-constructed software medical devices, we believe that stroke care will be one of the areas where advances in computer vision and deep learning will converge with clinical practice. Faster and more targeted stroke care delivers both economic and social benefits to society, as well as improved quality of life to stroke survivors.
Collaborate with us
We are interested in learning more from practicing clinicians and researchers about advances in stroke diagnostics and stroke care that are addressable by deep learning-enabled medical devices. To set up a conversation, please contact us.
References
[1] Camilo R. Gomez. Time Is Brain: The Stroke Theory of Relativity. Journal of Stroke and Cerebrovascular Diseases, 2018;27 (8): 2214 DOI: 10.1016/j.jstrokecerebrovasdis.2018.04.001
[3] https://www.heart.org/idc/groups/heart-public/@wcm/@mwa/documents/downloadable/ucm_501301.pdf
[4] Bhaskar, S., Stanwell, P., Cordato, D. et al. Reperfusion therapy in acute ischemic stroke: dawn of a new era?. BMC Neurol 18, 8 (2018). https://doi.org/10.1186/s12883-017-1007-y
[5] Pirson, F.A.V.(.A., Hinsenveld, W.H., Goldhoorn, RJ.B. et al. MR CLEAN-LATE, a multicenter randomized clinical trial of endovascular treatment of acute ischemic stroke in The Netherlands for late arrivals: study protocol for a randomized controlled trial. Trials22, 160 (2021). https://doi.org/10.1186/s13063-021-05092-0

Recent Comments